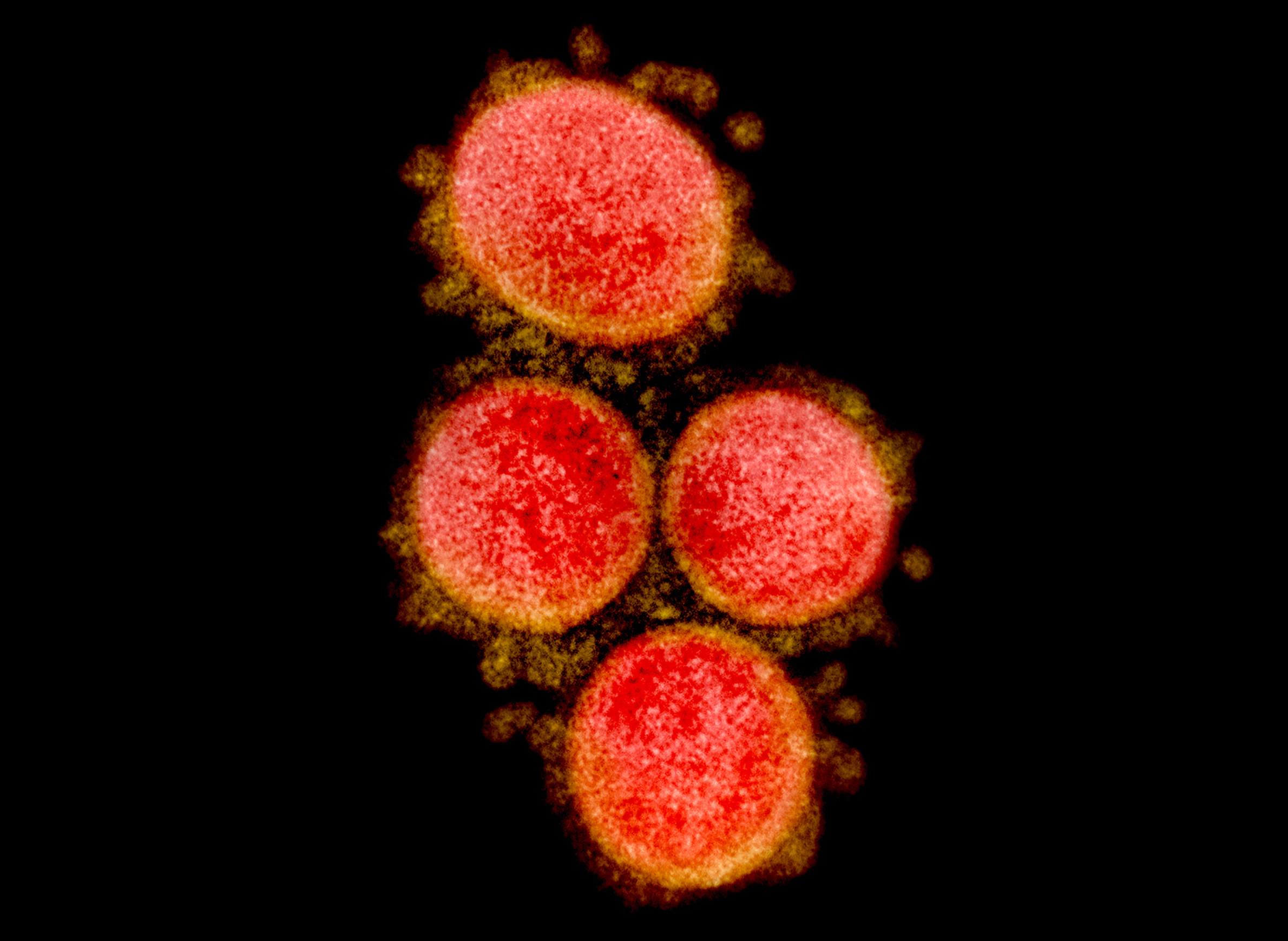
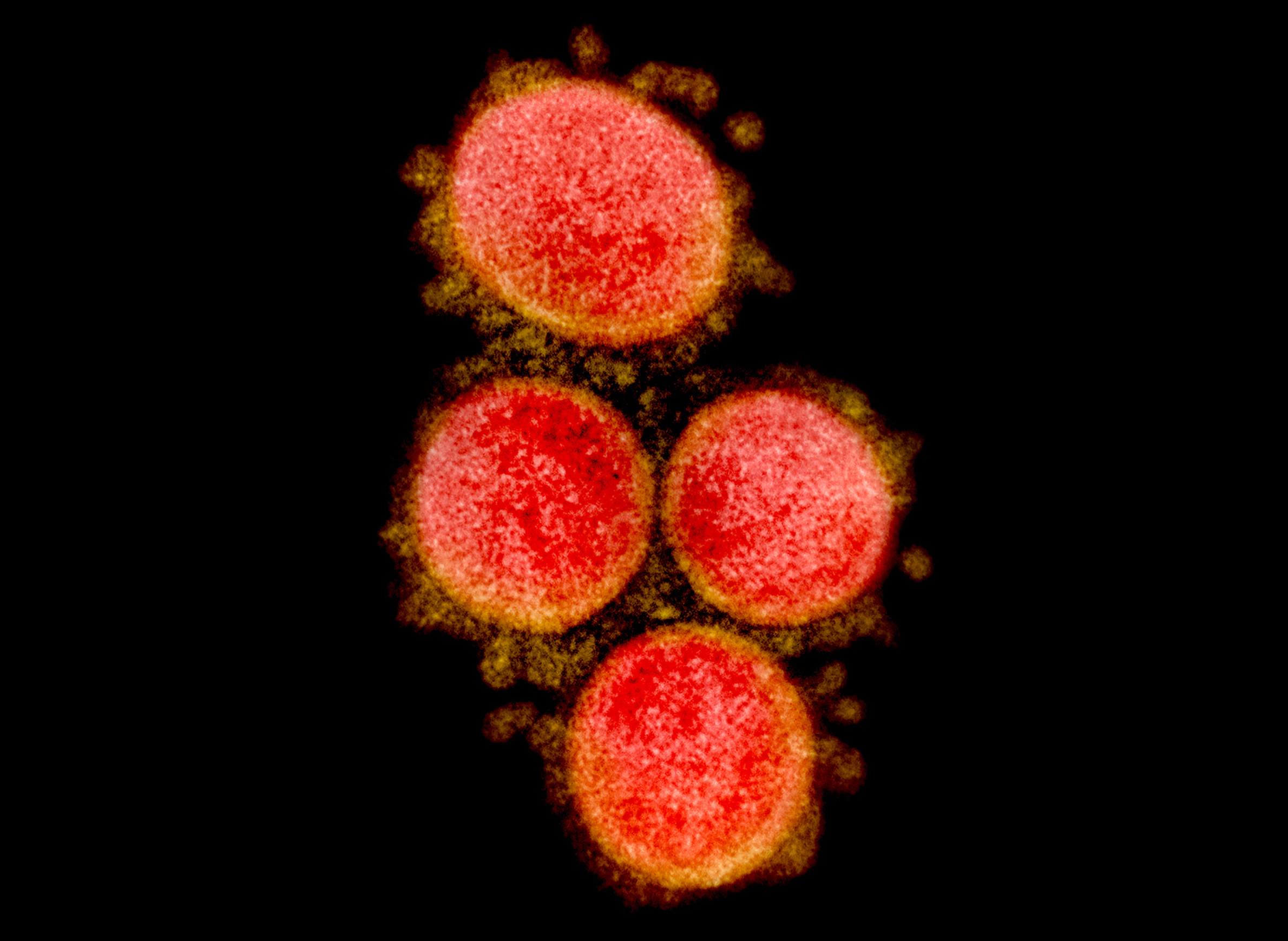
What The COVID-19 Pandemic Looks Like In Wisconsin: Maps And Charts
Editor's note: This article was originally published on April 1, 2020 and has since been updated, with the most recent changes made on Aug. 6, 2022. Data visualizations are updated on a recurring basis.
Following its emergence, the COVID-19 pandemic struck Wisconsin in a series of waves with varying degrees of intensity that has peaked multiple times. Click on the table of contents or swipe the page to view a series of visualizations that depict the impacts of COVID-19 across the state.
Introduction
Knowing the trajectory of COVID-19 in Wisconsin can help public health officials discern to what degree actions designed to slow its spread are needed and effective. Tracking these shifts can also help healthcare workers and hospital systems better prepare to care for patients.
Statewide cases and deaths
The state reports new confirmed infections and deaths reported on a daily basis. If the number of new confirmed cases rises day to day, that's a sign that the outbreak is growing. Fluctuations in daily deaths are a lagging indicator reflecting a preceding change in cases.
The goal of public health officials is for the number of new confirmed cases and deaths to fall over time. Since the period between coronavirus exposure and the onset of symptoms can be up to two weeks, and death in serious cases can follow long after infection, discernible effects of public health measures are delayed. A simple way to understand the short-term dynamics of an outbreak is to track a 7-day moving average of newly confirmed cases and deaths. The trend line of these moving averages is sensitive to fluctuating daily numbers, and can help indicate when an outbreak is surging, has peaked or is declining.
The total number of people in Wisconsin who have tested positive for COVID-19 and those who have died as a result are a longer-term metric of how the disease has affected the state. If cases and deaths are growing rapidly by the day, the pace of total infections and fatalities over time will have steep upward trajectories, while decreases in daily numbers leads to a flatter line.
The case fatality rate is another key COVID-19 metric. This measure reflects the percentage of confirmed cases that have resulted in a death attributed to the disease. However, it doesn't account for unconfirmed COVID-19 cases or unattributed excess deaths, and therefore carries uncertainties that may not reflect the disease's actual death rate.
County cases and deaths
The number of confirmed COVID-19 cases and deaths varies widely among Wisconsin's 72 counties. As the pandemic has continued, daily confirmed case and death counts at the county level accumulate and highlight regional patterns of COVID-19 infections. Given the widespread nature of COVID-19, a county-level map of total cases and deaths in large part reflects population density in the state.
County-level statistics about local COVID-19 outcomes are more informative when considered in terms of the size of the local population. Ten infections in a large, densely populated metro area with multiple hospitals is much different than 10 infections in a tiny community without a health clinic. It's therefore useful to evaluate local outbreaks relative to the size of local populations, commonly known as a per capita rate — in this case, confirmed cases or deaths per 100,000 residents.
County-level trends in COVID-19 transmission around Wisconsin can also be observed over time and through different types of groupings. Adjusting case rates to population size can provide further insight about the relative intensity of local spread. In this case, visualizing the growth in case rates over the course of the pandemic through a county's population sizes shows how COVID-19 affected different parts of the state as successive waves of infections were reported.
Recent cases
The near-term number of new confirmed COVID-19 cases in Wisconsin reflect the status of the pandemic at the present moment. One way to visualize recent confirmed COVID-19 cases across Wisconsin is to depict the per capita rates of confirmed cases in each county, with those over the previous 14 and 30 days depicting where outbreaks are spreading.
Testing
Widespread testing for COVID-19 provides another metric for understanding the spread of the disease. The total number of confirmed cases in Wisconsin is likely considerably smaller than the true number of infections. Many people who are infected may not show symptoms, and others with mild or moderate symptoms may not be tested. Still, understanding how many tests indicate infections provides a snapshot of the disease's prevalence at any given point in time.
A metric related to these efforts is the percent of tests that come back with positive results, which is known as a test-positivity rate. While the rate is subject to daily fluctuations, its longer-term trajectory can reveal how rapidly COVID-19 is spreading. Higher rates can indicate that testing strategies are missing many sick individuals, while a declining rate over time could indicate whether infections are coming under control.
There are multiple ways to calculate test-positivity rates. One common method is to divide the number of people who test positive by the number of people who are tested. Another method is to divide all positive tests by the total number of tests with results. The rates based on these two methods may diverge over time as a growing number of people receive repeat tests. Additionally, the number of tests performed each day is highly variable, which can lead to daily fluctuations in positivity rates. To better understand trends in positivity, rates are calculated based on moving 7-day periods.
Throughout much of the pandemic, the Wisconsin Department of Health Services calculated test-positivity by both tests and people. In February 2021, the agency dropped its calculations by people, citing a shrinking number of Wisconsinites who had never been tested. For comparison, an archived chart of the 7-day test-positivity average by people running from March 9, 2020 through Feb. 6, 2021 shows how this method of calculation can result in different daily figures. However, the different methods show parallel trends in test-positivity over time.
Before presenting these test-positivity calculations, WisContext calculated daily positivity rates and 7-day averages using data differently. In this case, the rates were based on test results on the day they were reported, rather than the subsequent method where rates reflected the date of the test result. Due to reporting lags, that previous method resulted in slightly different positivity rates, and WisContext ended its tracking of positivity with this method after Sept. 29, 2020 to align with the state health department's methods.
Hospitalizations
On a daily basis, the Wisconsin Hospital Association has tracked the number of total hospitalizations related to COVID-19 across the state, as well as more specific metrics related to the use and availability of intensive care unit beds. It also presents these figures for the state's seven healthcare readiness regions — coalitions of hospital networks that coordinate resources — metrics that have been used by public health officials to gauge regional differences in capacity. These figures show the breadth of the disease's impact on Wisconsin's hospitals by accounting for discharges and regional differences.
If public health measures designed to slow the spread of COVID-19 have an effect, and the number of new cases begins to fall, a plot of total infections over time would become less steep, or flatten. It's the origin of the ubiquitous term "flattening the curve" in discussions about COVID-19.
Flattening the curve is primarily aimed at protecting the capacity of healthcare systems to treat serious cases of COVID-19 while maintaining other essential care. A relatively small but significant number of cases are serious enough to warrant hospitalization, with the most serious requiring intensive care.
Demographics
As is the case across the United States, Wisconsin has seen demographic disparities in the number and severity of COVID-19 cases, hospitalizations and deaths, as well as the distribution of vaccines. One of the primary risk factors is increasing age, which is evident from statewide data showing the risk for each by 10 different age groups.
Reflecting national patterns, Wisconsin has also seen disparities in COVID-19 cases, hospitalizations and deaths based on racial and ethnic classifications. Data show that some groups, including Indigenous, Black and Hispanic Wisconsinites, are diagnosed with COVID-19 at higher rates than white Wisconsinites. Indigenous and Black Wisconsinites have also been hospitalized and died due to the disease at higher rates. There are also racial and ethnic disparities in the rate of vaccination.
Vaccinations
The first COVID-19 vaccines were delivered to Wisconsin in December 2020, and healthcare workers embarked on a long and complex effort to vaccinate as many state residents as possible. Wisconsin received regular allocations of COVID-19 vaccine doses from the federal government, with the number provided based on population and supplies available from manufacturers. Healthcare systems, pharmacies and other vaccine providers in the state made requests for doses, and the Wisconsin Department of Health Services factored those requests into its requests to the U.S. Department of Health and Human Services.
The administration of COVID-19 vaccines to Wisconsin residents has been incremental, with distinct geographic differences in their use around the state. Vaccination is authorized for individuals ages 6 months and older, which represents nearly all of the state's total population of more than 5.8 million people.
COVID-19 vaccines produced by Pfizer and Moderna require two doses that are administered several weeks apart. The vaccine produced by Johnson & Johnson requires only one dose. The state therefore tracks not only the daily number of doses but likewise the total number of people in Wisconsin who have completed their vaccine series, statewide and at the county level. Scientists have estimated that upward of 70% of the population needs to be vaccinated to effectively limit the spread of the coronavirus and halt the pandemic.


