Strokes Call For Fast Reactions
With a rapidly aging population, public awareness of strokes, their causes and their symptoms is becoming more important. As the Wisconsin Coverdell Stroke Program has detailed, strokes were the state's fifth leading cause of death in 2016. Strokes killed about 2,500 people in the state that year, while in 2017 some 11,000 hospitalizations were attributed to the malady. Every year, thousands of Wisconsinites suffer strokes and dealt with long-term damage to their brains and bodies.
The symptoms and causes of strokes can vary widely, but it's always crucial to get victims medical help as quickly as possible. Justin Sattin, an associate professor of neurology at the University of Wisconsin School of Madison and Public Health, explained the importance of haste in spotting and treating strokes in an April 16, 2015 talk recorded for Wisconsin Public Television's University Place.
Sattin presented the basics of why strokes happen, how they affect the brain, and the different problems in the body that bring them about. He also discussed what individuals should do if they or someone they know is having stroke symptoms, and detailed the challenges of diagnosing and treating strokes as rapidly as needed.
The American Stroke Association tries to help people identify strokes with the acronym FAST: face drooping, arm weakness, speech difficulty and time (as in time to call 911). The Wisconsin Coverdell Stroke Program, which is a program of the Centers for Disease Control and Prevention, uses a similar mnemonic to emphasize the need for quickly recognizing and acting on the signs of strokes.
Distance creates one major difficulty in addressing strokes quickly and effectively. Large portions of Wisconsin are more than an hour's drive away from a medical facility certified to treat strokes. In such areas, emergency room doctors often end up seeking guidance by phone from stroke specialists.
Health care providers have tried to improve upon this problem by letting stroke specialists consult with patients and local doctors and nurses via telemedicine, with help from a remote-controlled camera. For example, UW doctors have expanded the use of this technology via an effort known as the UW Telestroke Network. It allows specialists to conduct detailed examinations with stroke victims and/or their family members, speeding efforts by local emergency rooms and clinics to provide care.
Key facts
- A stroke is an interruption to the flow of blood to the brain, causing damage or death to sections of brain tissue.
- Symptoms of a stroke include numbness or weakness on one side of the body, confusion or difficulty speaking, difficulty hearing, difficulty maintaining balance, severe headaches, drooping in the face and vision loss in one or both eyes.
- Speech problems during a stroke can include slurring, not being able to make the right words come out, or difficulty understanding the speech of others. The sudden onset of these problems is the common factor.
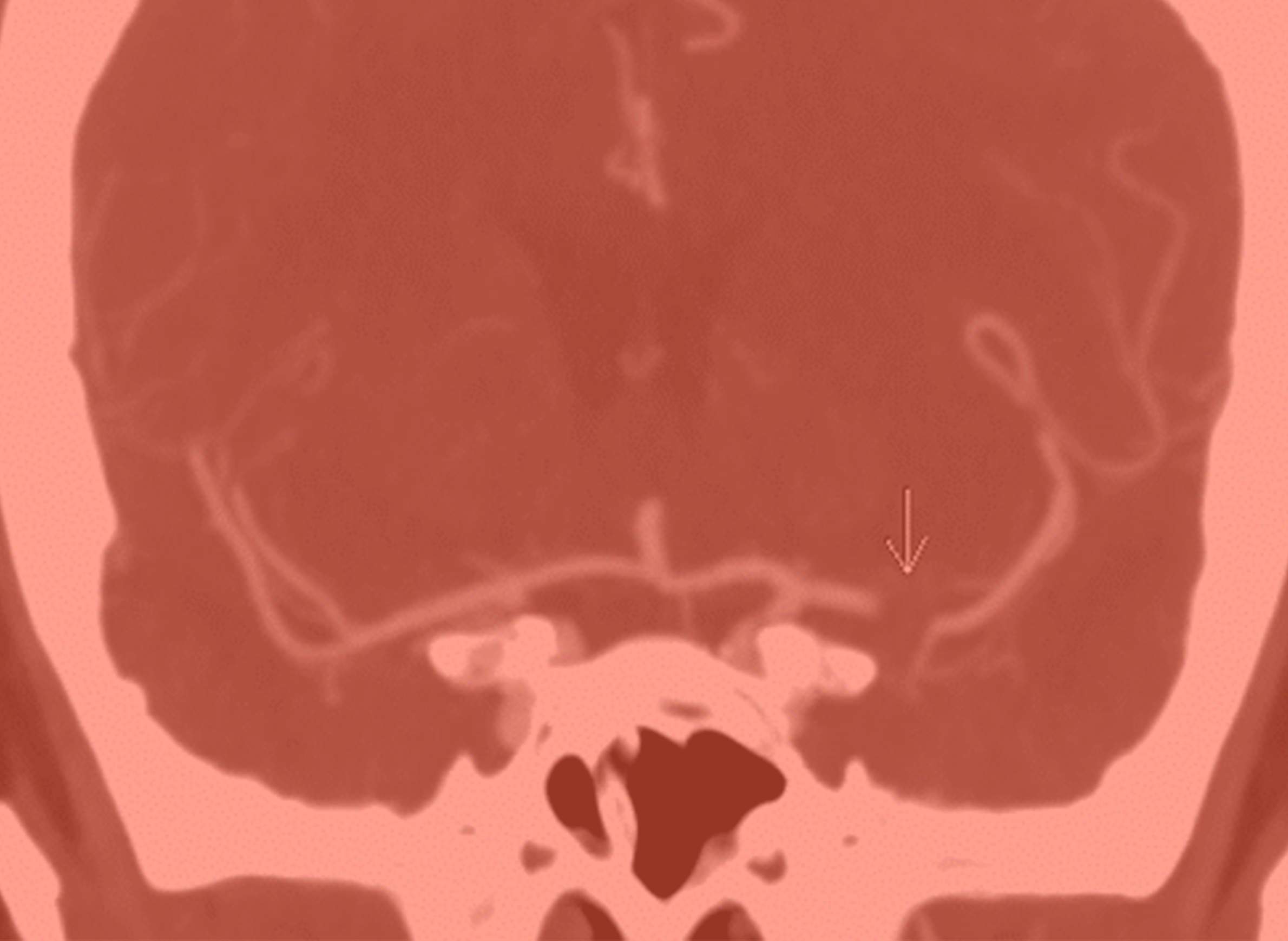
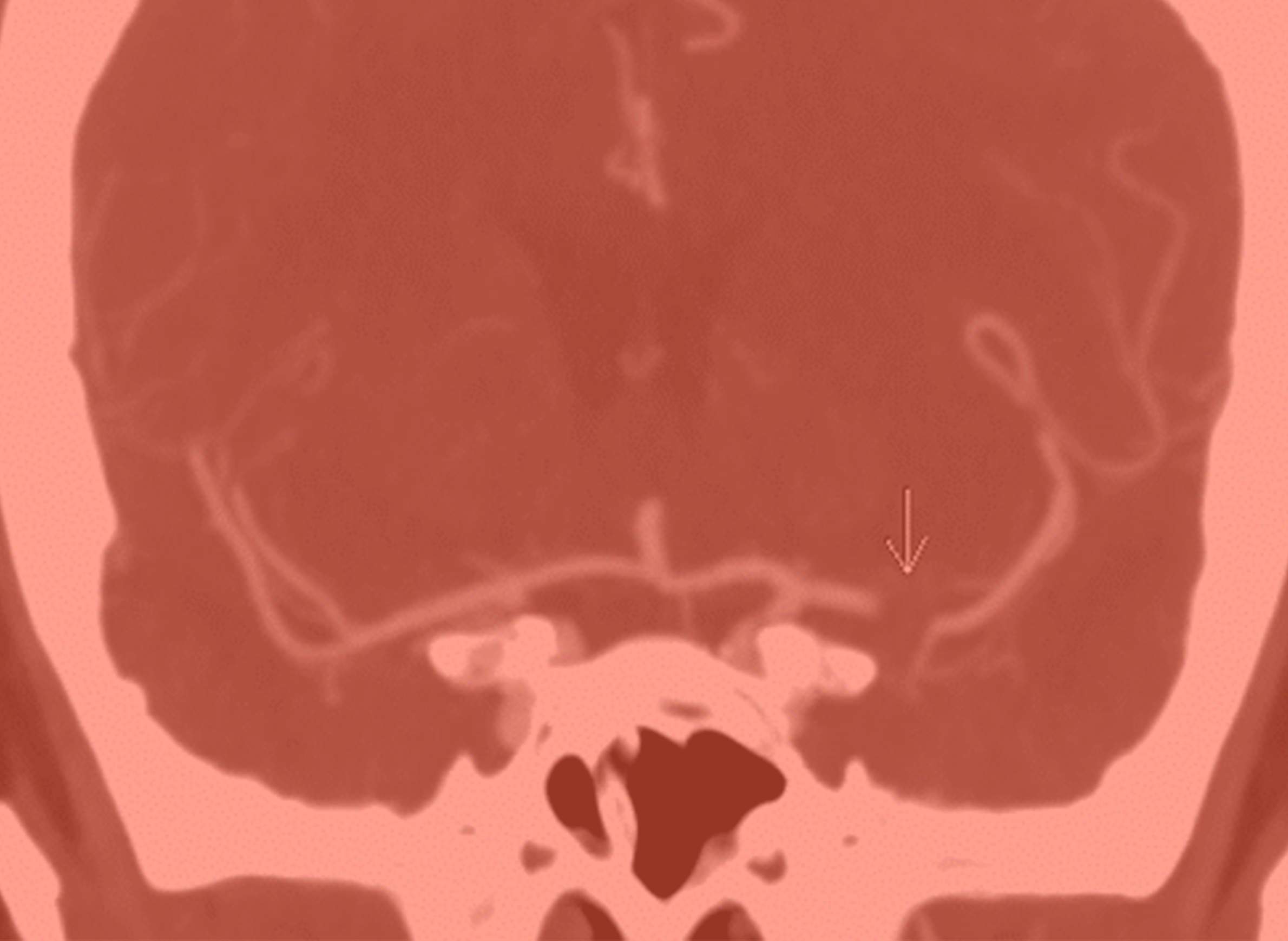
- There are two main categories of stroke. An ischemic stroke occurs when plaque or a blood clot becomes lodged in the brain's arteries and obstructs that blood flow. A hemorrhagic stroke occurs when arteries rupture, causing blood to spill into brain tissue.
- About 80 percent of strokes are ischemic and 20 percent are hemorrhagic. Because ischemic strokes are more common, there are more treatments for them than for hemorrhage strokes.
- Ischemic strokes have multiple causes, often related to heart problems, including atrial fibrillation. In this disorder, an irregular quivering of the heart allows blood moving through the heart to clot. Carotid artery disease, in which plaque builds up in one of the major arteries serving the brain, is another major contributor. Plaque can also build up in arteries deep inside the brain itself, in a condition known as intracranial artery disease.
- Hemorrhagic strokes likewise have a variety of causes. Blood vessels can develop weaknesses at points where they branch off within the brain, causing what's known as a subarachnoid hemorrhage. But in most cases, hemorrhage strokes occur when tiny arteries burst deep within the brain tissue.
- MRI scans can identify the damage to the brain after a stroke, and can provide insight into its cause. Different patterns of injury in the brain can help doctors better understand, for instance, where the clots or plaque causing the stroke originated. People suffering from arterial problems can have surgical procedures that are intended to prevent a stroke.
- It's important for stroke victims to note the time of onset, because treatments are tailored to how long the stroke has been happening. For instance, the drug tPA is most effective within the first hour of a stroke, and the U.S. Food and Drug Administration only approves its use up to three hours in an episode.
- Other treatments for strokes involve running catheters up through patients' arteries and into the brain, using small tools mounted on them to remove obstructions to blood flow. However, only a minority of stroke victims qualify for this treatment.
Key quotes
- On recognizing strokes: "One key to all this is that it's sudden. So people who develop numbness that progresses over time are not having a stroke. Stroke is when you're totally fine, and then, boom, suddenly something happens because the artery was open and now it's not open, it's obstructed with a clot. Or the artery was just fine and then, boom, it suddenly ruptures and blood starts spilling out into the brain."
- On what to do when having stroke symptoms: "So the thing to do is to call 911, and not your daughter who happens to be a nurse and not your doctor who's going to call you back a couple hours later after you leave a message or something. You have to call 911. You have to call 911. It's very important … if you start burning your minutes and hours by making various phone calls or maybe I just need to get something to eat or take a nap or I'll wait for my spouse to get home or I'll put in a call to my primary, after all he knows me for 30 years, you're just burning through your time, and by the time somebody figures out that you might be having a stroke and you got to get to the emergency room, [it's] too late."
- On the difficulties of identifying strokes and educating the public about them: "It's not like a heart attack where it's basically chest pain. Everybody knows chest pain, you need to think about heart attack. And there's a few nuances to that, and the pain can radiate down the left side and into the jaw, but you know that whole thing is pretty well known. Whereas stroke is more difficult because there's so many different things that a stroke can do, and you need to be able to recognize all of them or at least know that when there's a sudden onset of some neurological problem, that stroke may be the cause."
- On distinguishing one kind of stroke from another based on symptoms: "There may be some subtle clues. For example, if there's a severe headache, that would suggest more that there's brain hemorrhage. You've got something taking up space inside the head so that hurts. But about 20 percent of ischemic strokes have headache associated too, so you can't use that as a definitive way to differentiate them."
- On the difficulty of helping other doctors treat strokes over the phone: "As you might imagine, there's some degradation of the information. The ER doc is telling me that his radiologist told him that the CAT scans shows X, Y or Z. Or you get an emergency room doc who might be a very good emergency room doc, but he's not a neurologist. And so for me to try to figure out what exactly are the neurological findings and so forth can be difficult to make recommendations about whether to give tPA or not, whether the patient needs to be transferred to a tertiary care center or not."



